An “electronic nose” analyzes people’s breath to help sniff out diseases
In partnership with IMT Atlantique, a team of researchers at IMT Lille Douai have developed a device which can measure the level of ammonia in someone’s breath. The aim of the artificial nose is to use this device to create a personalized follow-up care for patients affected by chronic kidney disease. Eventually, the machine could even allow doctors to detect the disease in undiagnosed people.
This article is part of our dossier “When engineering helps improve healthcare“
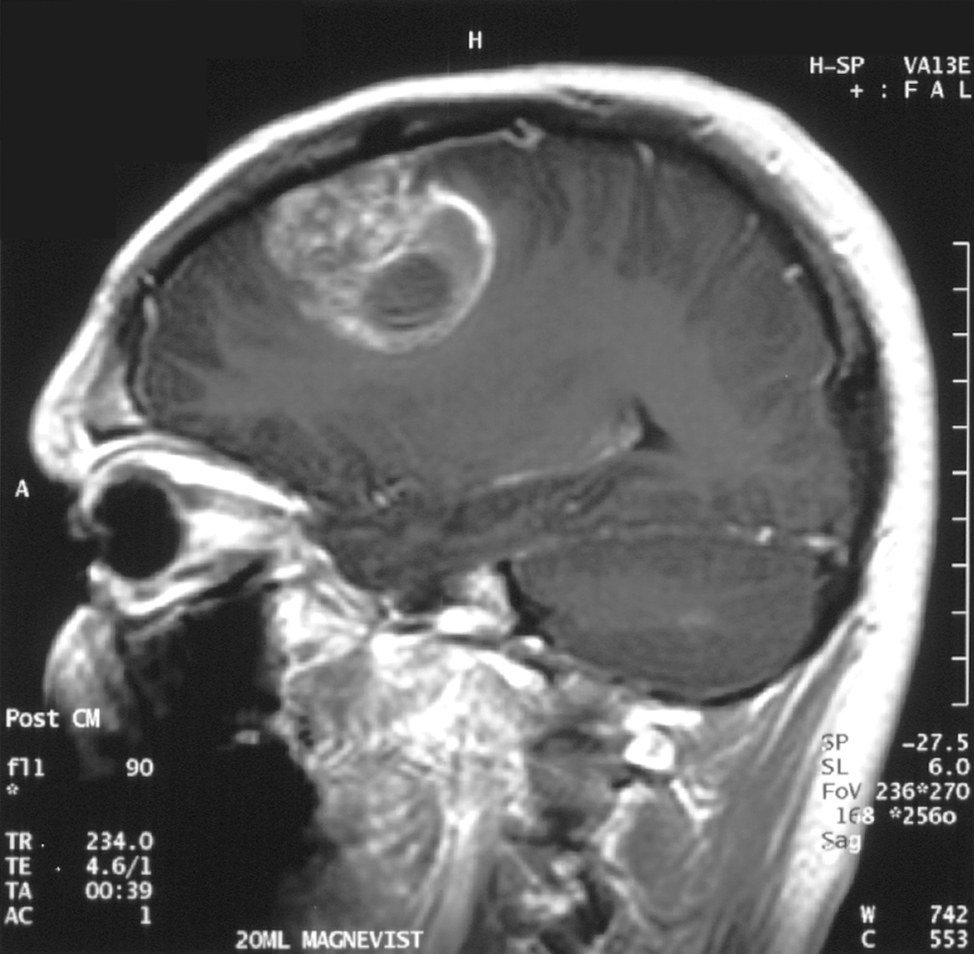
In the human body, the kidneys’ main role is to remove toxins which are carried in the blood. However, when a person suffers from chronic kidney disease, this filtration function no longer works to the same standard. In France, the disease affects around 5.7 million people and can range from causing a degree of impairment, to terminal. Around 76,000 people are terminally affected in France, which means that their kidneys cannot filter their blood at all.
For these patients, the only options are to either wait for a transplant or face extensive treatment which hugely affects their daily life. It is therefore essential for doctors to be able to detect this silent and progressive disease early enough to slow down the effects. At the moment, doctors use blood or urine tests to identify the disease. But, to make it easier to diagnose, scientists are exploring another route: breath analysis. Studying the substances in the air we breathe out can provide valuable information about a person’s health.
Ammonia: a key element
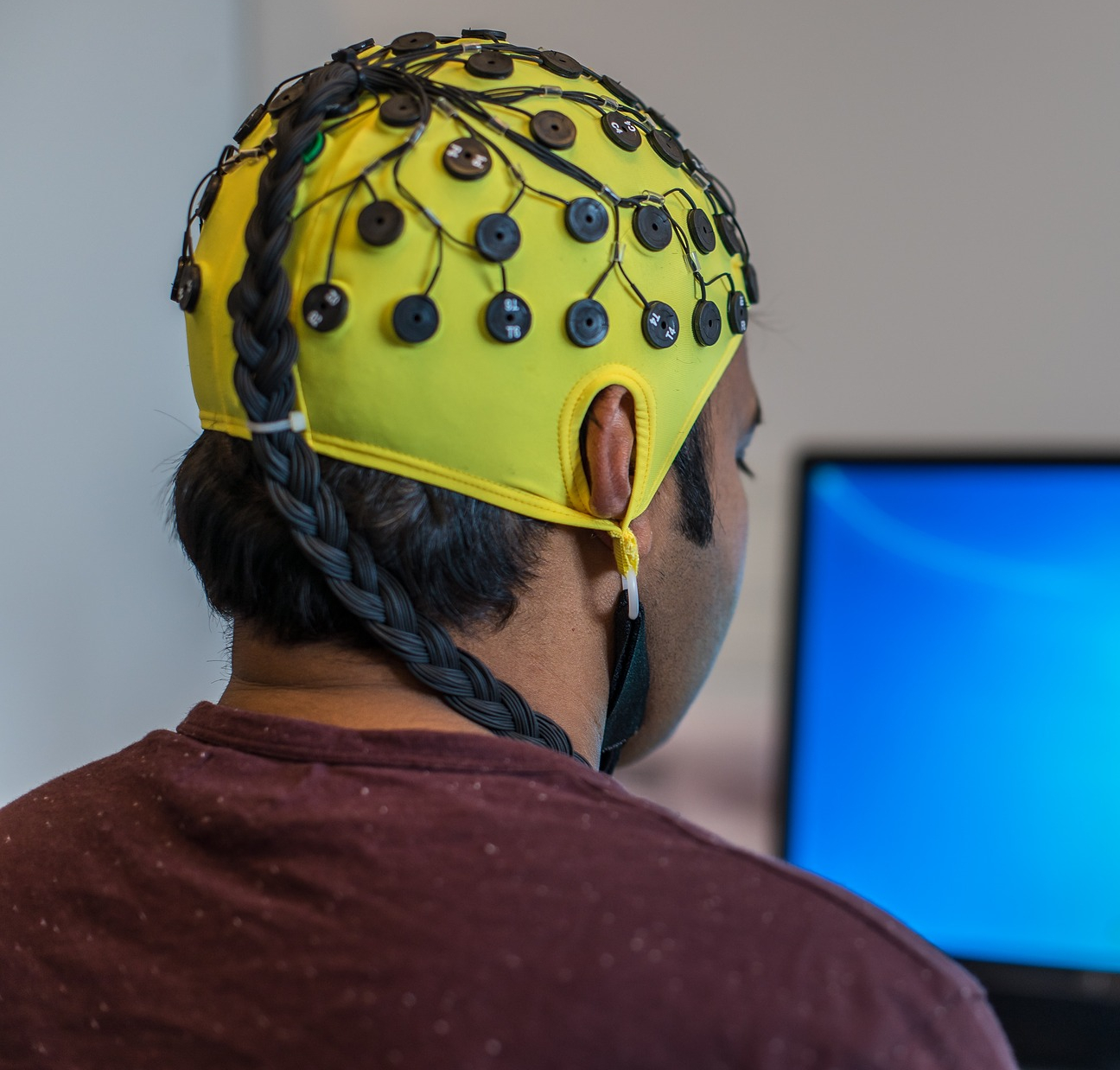
In order to make this possible, two teams of researchers from IMT Lille Douai and IMT Atlantique have been working in partnership with the nephrology department at the Lille University Hospital. For the past three years, they have been developing a compact and turnkey device for doctors. The device is an ‘electronic nose’, a system made up of several sensors that can measure the specific concentration of a substance in someone’s breath.
In the case of chronic kidney disease, the substance being measured is ammonia. Ammonia is mainly produced by intestinal bacteria and is supposed to be filtered from the body by the kidneys. Previous studies have established a concentration threshold for levels of ammonia in a person’s breath, which doctors can then use to determine the likelihood that a patient has chronic kidney disease.
Ammonia offers some resistance
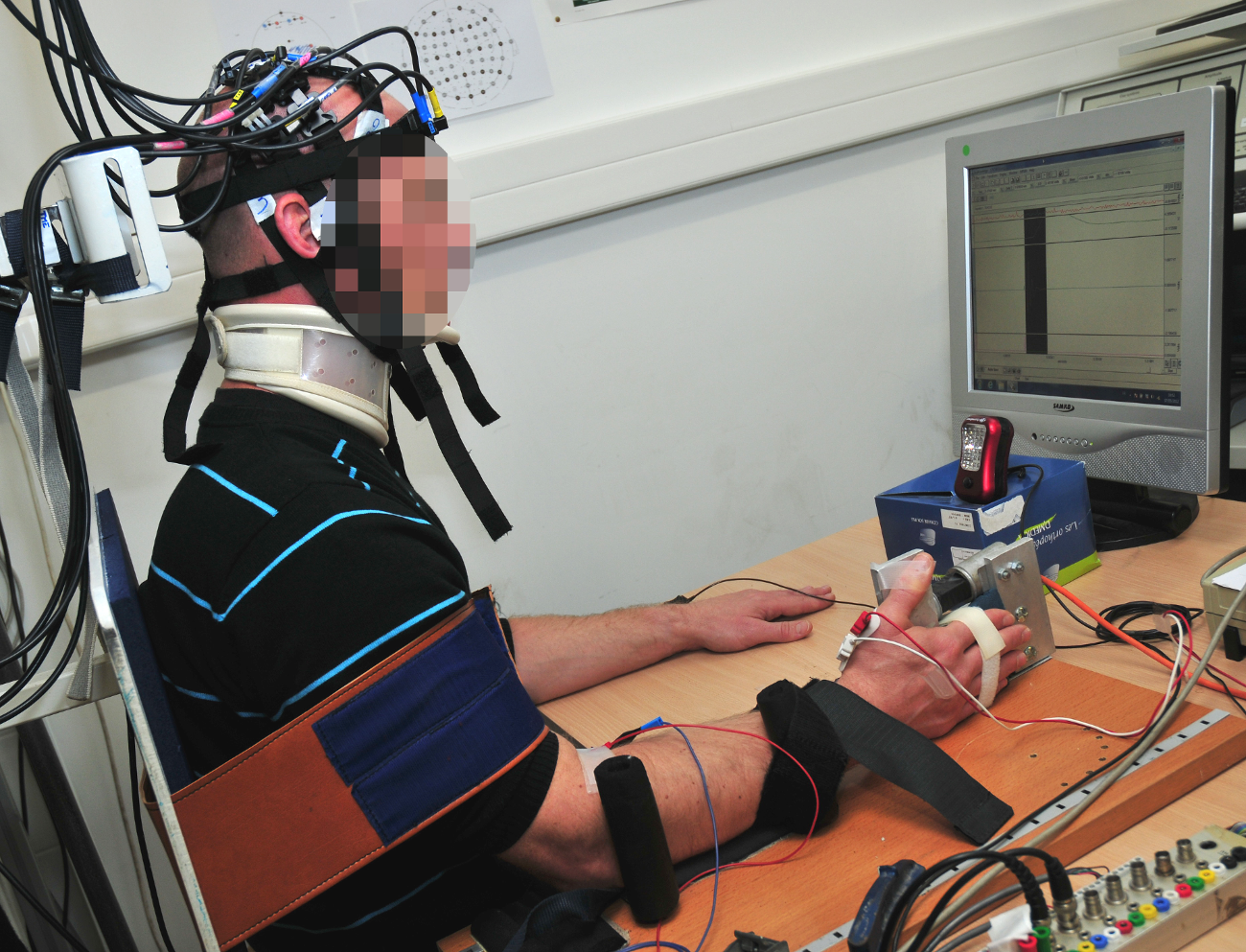
But how can you measure this compound using a portable device? The scientists used a series of sensors which react in the presence of ammonia, as Caroline Duc, team member and researcher at IMT Lille Douai, explains. “The sensors are made from two electrodes with a sensitive surface placed on top of them. The resistance of this surface varies depending on the amount of ammonia present”. When used, the device’s ability to resist electrical current increases when ammonia is present and returns to its initial state when the ammonia disappears. This therefore allows scientists to measure the level of the molecule in a patient’s breath.
Additionally, each sensor in the artificial nose has a unique composition. As Caroline Duc points out, “it is very complicated to use a material whose resistance varies when one type of gas is present”. This is why scientists decided to increase the accuracy of the analysis by combining several different sensors which have different responses to ammonia.
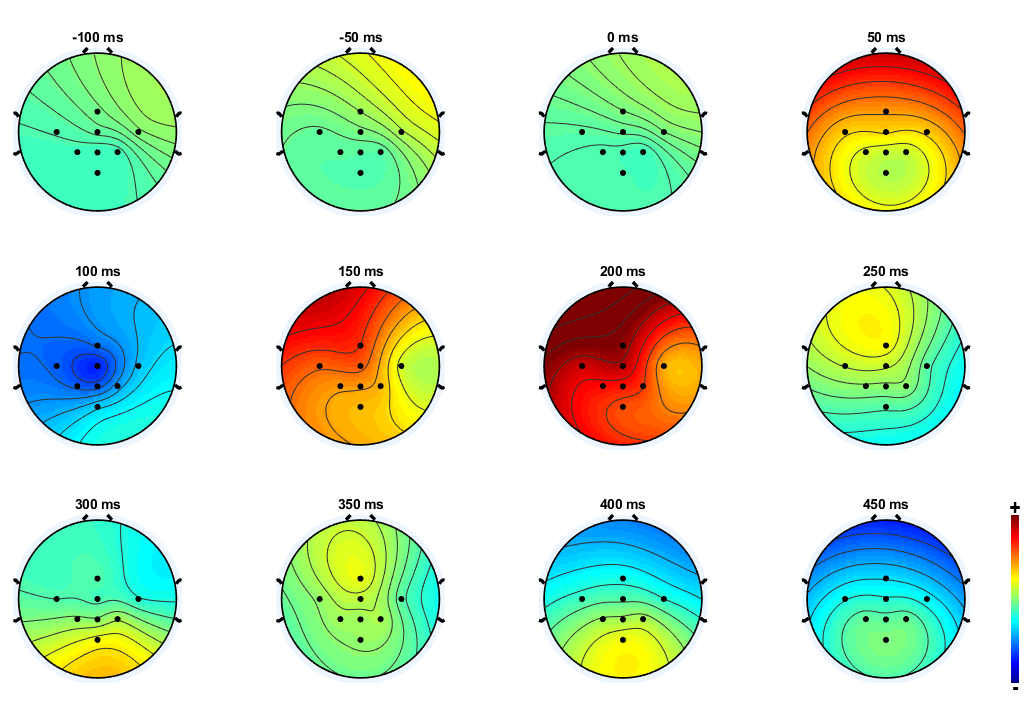
During the tests, the electronic nose was periodically exposed to a person’s breath. This resulted in an increase in the resistance when ammonia was present, and a decrease when the sensors were no longer exposed to the exhaled air. Several factors were then measured and analyzed using statistical processing algorithms.
These algorithms rely on tools such as machine learning. The only difference with this case was that here, these tools were applied using small amounts of data and supervised learning to categorize the different types of breath. In other words, the algorithms were taught using a dataset that had already classified breath which belongs to a healthy, ill or ‘uncertain’ individual. New profiles were then passed through this algorithm, so that they could be classed into these three categories.
Breath: a complex compound
To date, the first prototype developed is around 15cm in length and contains between 10 and 13 sensors. The device was tested in a laboratory using artificial breath, which allowed the teams to verify that it could distinguish a healthy individual from someone who was ill, using the criteria defined in up-to-date scientific literature. Then, experiments were carried out in clinics with patients suffering from chronic kidney disease. The idea was to measure the concentration of ammonia in their breath, before and after dialysis. The results demonstrated that there was a reduction in ammonia after the treatment.
However, they also highlighted the limitations of using a single marker. Before dialysis, some patients had levels of ammonia that were similar to those of a healthy person. Measuring the amount of ammonia in a person’s breath did not give a reliable diagnosis for chronic kidney disease. This has caused scientists to launch a new study in order to identify other biomarkers characteristic of the disease.
More generally, this reflects the difficulty of conducting a reliable breath analysis, which can include both the air we breathe in as well as out. “Initially, I think clinical breath analysis will be developed for personalized patient follow-up care, rather than for diagnosis”, says Caroline Duc. For example, by measuring how a patient’s ammonia levels change in response to medication, doctors will be able to monitor the effectiveness of a treatment and then adapt it based on the results.
What is the future of follow-up care for other illnesses?
Researchers at IMT Lille Douai will continue to work on improving the electronic nose. At the moment, patients’ breath is collected and sealed in an airtight bag and is then analyzed in a laboratory. Consequently, the team’s aim is to develop a functional and completely autonomous prototype which would give doctors real-time results. However, this raises several new issues, such as the study of fluids, controlling the speed that the air is exhaled, etc. As well as this, to improve their data analysis, Caroline Duc and her colleagues have started a partnership with researchers who specialize in data handling at Télécom SudParis.
Moreover, the team is involved in a European-wide project which aims to identify biomarkers for lung cancer, and then create a multi-sensor system that is specifically designed to detect these substances. IMT Lille Douai’s expertise will be especially useful for this second objective.
This electronic nose, capable of sniffing out illnesses such as chronic kidney disease, is therefore still in the early stages of development, and needs a lot of work before it can really be used by doctors and their patients. But doctors are waiting with bated breath; in several years’ time it could be a breathtaking medical innovation!
Article written (in French) for I’MTech by Bastien Conteras